What is it?
- Cholera is a bacterial disease usually spread through contaminated water. Cholera causes severe diarrhoea and dehydration. Left untreated, cholera can be fatal in a matter of hours.
- Modern sewage and water treatment have virtually eliminated cholera in industrialized countries. But cholera is still present in Asia, the Middle East, Latin America, India and sub-Saharan Africa. The risk of cholera epidemic is highest when poverty, war or natural disasters force people to live in crowded conditions without adequate sanitation.
- Cholera is easily treated.
Symptoms
Most people exposed to the cholera bacterium (called Vibrio cholerae) don't become ill and never know they've been infected. Yet because they shed cholera bacteria in their stool for seven to 14 days, they can still infect others. Most symptomatic cases of cholera cause mild or moderate diarrhea that's often hard to distinguish from diarrhea caused by other problems.
Only about one in 10 infected people develops the typical signs and symptoms of cholera, which include:
- Severe, watery diarrhoea. The incubation time for cholera is brief — usually one to five days after infection. Diarrhea comes on suddenly. Diarrhea due to cholera is often voluminous, flecked with mucus and dead cells, and has a pale, milky appearance that resembles water in which rice has been rinsed (rice-water stool). What makes cholera diarrhea so deadly is the loss of large amounts of fluids in a short time — as much as a quart (.95 liters) an hour.
- Nausea and vomiting. Occurring in both the early and later stages of cholera, vomiting may persist for hours at a time.
- Muscle cramps. These result from the rapid loss of salts such as sodium, chloride and potassium.
- Dehydration. This can develop within hours after the onset of cholera symptoms — far more quickly than in other diarrheal diseases. Depending on how much body fluids have been lost, dehydration can range from mild to severe. A loss of 10 percent or more of total body weight indicates severe dehydration. Signs and symptoms of cholera dehydration include irritability, lethargy, sunken eyes, a dry mouth, extreme thirst, dry, shriveled skin that's slow to bounce back when pinched into a fold, little or no urine output, low blood pressure, and an irregular heartbeat (arrhythmia).
- Shock. Hypovolemic shock is one of the most serious complications of cholera dehydration. It occurs when low blood volume causes a drop in blood pressure and a corresponding reduction in the amount of oxygen reaching your tissues. If untreated, severe hypovolemic shock can cause death in a matter of minutes.
Signs and symptoms of cholera in children
In general, children with cholera have the same signs and symptoms adults do, but they may also experience:
- Extreme drowsiness or even coma
- Fever
- Convulsions
Causes
- Contaminated water supplies are the main source of cholera infection, although raw shellfish, uncooked fruits and vegetables, and other foods also can harbor cholera bacteria.
- The bacterium that causes cholera, Vibrio cholerae, has two distinct life cycles - one in the environment and one in humans.
Cholera bacteria in the environment
Cholera bacteria occur naturally in coastal waters, where they attach to tiny crustaceans called copepods. As many as 10,000 bacteria may adhere to a single crustacean. The cholera bacteria travel with their hosts, spreading worldwide as the crustaceans follow their food source - certain types of algae and plankton that grow explosively when water temperatures rise. Algae growth is further fueled by the urea found in sewage and in agricultural runoff.
Most cholera outbreaks occur in spring and fall when ocean surface temperatures and algae blooms are at their height. More algae mean more copepods, and more copepods mean more cholera bacteria.
Cholera bacteria in people
When humans ingest cholera bacteria, they may not become sick themselves, but they still excrete the bacteria in their stool and can pass cholera disease to others through the fecal-oral route. This mainly occurs when human feces contaminate food or water supplies, both of which can serve as ideal breeding grounds for the cholera bacteria. Because more than a million cholera bacteria - approximately the amount you'd find in a glass of contaminated water - are needed to cause illness, cholera usually isn't transmitted through casual person-to-person contact.
The most common sources of cholera infection include:
- Surface or well water. Cholera bacteria can lie dormant in water for long periods, and contaminated public wells are frequent sources of large-scale cholera outbreaks. Cholera epidemics are most likely to occur in communities without adequate sanitation and in areas affected by natural disasters or war. People living in crowded refugee camps are especially at risk of cholera.
- Seafood. Eating raw or undercooked seafood, especially shellfish, that originates from certain locations can expose you to cholera bacteria. Most cases of cholera occurring in the United States since the 1970s have been traced to oysters and crab from the Gulf of Mexico and to seafood transported or smuggled from countries where cholera is endemic. Shellfish are a particular problem because they filter large amounts of water, concentrating the levels of cholera bacteria.
- Raw fruits and vegetables. Raw, unpeeled fruits and vegetables are a frequent source of cholera infection in areas where cholera is endemic. In developing nations, uncomposted manure fertilizers or irrigation water containing raw sewage can contaminate produce in the field. Fruits and vegetables may also become tainted with cholera bacteria during harvesting or processing.
- Grains. In regions where cholera is widespread, grains such as rice and millet that are contaminated after cooking and allowed to remain at room temperature for several hours become a medium for the growth of cholera bacteria.
Bacteria produce strong toxin
Although V. cholerae is the source of cholera infection, the deadly effects of the disease are the result of a potent toxin, called CTX, that the bacteria produce in the small intestine. CTX binds to the intestinal walls, where it interferes with the normal flow of sodium and chloride. This causes the body to secrete enormous amounts of water, leading to diarrhea and a rapid loss of fluids and salts (electrolytes).
Risk factors
Everyone is susceptible to cholera, with the exception of infants who derive immunity from nursing mothers who have previously had cholera. Still, certain factors can make you more vulnerable to the disease or more likely to experience severe signs and symptoms. Risk factors for cholera include:
- Malnutrition. Malnutrition and cholera are interconnected. People who are malnourished are more likely to become infected with cholera, and cholera is more likely to flourish in places where malnutrition is common, such as refugee camps, impoverished countries, and areas devastated by famine, war or natural disasters.
- Reduced or nonexistent stomach acid (hypochlorhydria or achlorhydria). Cholera bacteria can't survive in an acidic environment, and ordinary stomach acid often serves as a first-line defense against infection. But people with low levels of stomach acid lack this protection, so they're more likely to develop cholera and to have severe signs and symptoms of the disease. Children and older adults, especially, tend to have lower than normal stomach acid levels. So do people who have had gastric surgery, who have untreated Helicobacter pylori infection, or who are taking antacids, H-2 blockers or proton pump inhibitors for ulcers. Antacids help neutralize stomach acid, and H-2 blockers and proton pump inhibitors reduce the amount of acid your stomach produces.
- Household exposure. You're at significantly increased risk of cholera if you live with someone who has the disease.
- Compromised immunity. If your immune system is compromised for any reason, you're more susceptible to cholera infection.
- Type O blood. For reasons that aren't entirely clear, people with type O blood are twice as likely to develop cholera as are people with other blood types.
- Raw or undercooked shellfish. Although large-scale cholera outbreaks no longer occur in industrialized nations, eating raw shellfish — particularly oysters — from waters known to harbor the bacteria or shellfish transported by travelers from countries where cholera is endemic greatly increases your risk.
Complications
Cholera can quickly become fatal. In the most severe cases, the rapid loss of large amounts of fluids and electrolytes can lead to death within two to three hours. In less extreme situations, people who don't receive treatment may die of dehydration and shock 18 hours to several days after cholera symptoms first appear.
Although shock and severe dehydration are the most devastating complications of cholera, other problems can occur, such as:
- Low blood sugar (hypoglycemia). A common cholera complication in children, hypoglycemia occurs when blood levels of glucose, the body's main energy source, fall abnormally low. Glucose is absorbed directly into your bloodstream after eating and enters your cells through the action of the hormone insulin. With severe cholera, people can become too ill to eat, so they don't get glucose from food. This may lead to unusually low blood sugar levels, which can cause seizures, unconsciousness and even death.
- Low potassium levels (hypokalemia). People with cholera lose large quantities of minerals, including potassium, in their stools. Very low potassium levels interfere with heart and nerve function and are life-threatening. Hypokalemia is especially serious in people whose potassium stores have already been depleted by malnutrition.
- Kidney (renal) failure. When the kidneys lose their filtering ability, excess amounts of fluids, some electrolytes and wastes build up in your body — a potentially life-threatening condition. In people with cholera, kidney failure often accompanies shock.
Diagnosis
Although signs and symptoms of severe cholera may be unmistakable in endemic areas, the only way to confirm a diagnosis is to identify the bacteria in a stool sample.
Rapid cholera dipstick tests are now available, enabling health care providers in remote areas to confirm diagnosis of cholera earlier. Quicker confirmation helps to decrease death rates at the start of cholera outbreaks and leads to earlier public health interventions for outbreak control.
Treatments and drugs
Cholera requires immediate treatment because the disease can cause death within hours.
- Rehydration. The goal is to replace fluids and electrolytes lost through diarrhea using a simple rehydration solution, Oral Rehydration Salts (ORS), that contains specific proportions of water, salts and sugar. The ORS solution is available as a powder that can be reconstituted in boiled or bottled water. Without rehydration, approximately half the people with cholera die. With treatment, the number of fatalities drops to less than 1 percent.
- Intravenous fluids. During a cholera epidemic, most people can be helped by oral rehydration alone, but severely dehydrated people may also need intravenous fluids.
- Antibiotics. Recent studies show that a single dose of azithromycin (Zithromax) in adults or children with severe cholera helps shorten diarrhea duration and decreases vomiting.
- Zinc supplements. Research has shown that zinc may decrease and shorten the duration of diarrhea in children with cholera.
Prevention
If you're traveling to cholera-endemic areas, your risk of contracting the disease is extremely low if you follow these precautions:
Wash your hands. Frequent hand washing is the best way to control cholera infection. Wash your hands thoroughly with hot, soapy water, especially before eating or preparing food, after using the toilet, and when you return from public places. Carry an alcohol-based hand sanitizer for times when water isn't available.
Avoid untreated water. Contaminated drinking water is the most common source of cholera infection. For that reason, drink only bottled water or water you've boiled or disinfected yourself. Coffee, tea and other hot beverages, as well as bottled or canned soft drinks, wine and beer, are generally safe. Carefully wipe the outside of all bottles and cans before you open them and ask for drinks without ice. Use bottled water to brush your teeth.
Eat food that's completely cooked and hot. Cholera bacteria can survive on room temperature food for up to five days and aren't destroyed by freezing. It's best to avoid street vendor food, but if you do buy it, make sure your meal is cooked in your presence and served hot.
Avoid sushi. Don't eat raw or improperly cooked fish and seafood of any kind.
Be careful with fruits and vegetables. When you're traveling, make sure that all fruits and vegetables that you eat are cooked or have thick skins that you peel yourself. Avoid lettuce in particular because it may have been rinsed in contaminated water.
Be wary of dairy foods. Avoid ice cream, which is often contaminated, and unpasteurized milk.
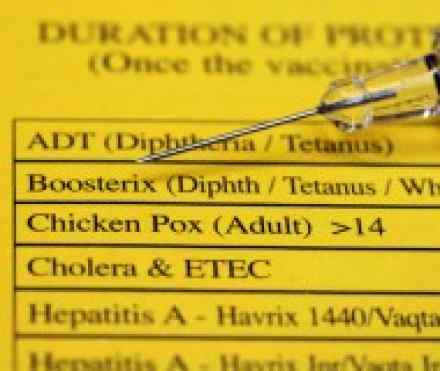
Cholera vaccine. Because travelers have a low risk of contracting cholera and because the traditional injected vaccine offers minimal protection, no cholera vaccine is currently available in the United States. A few countries offer two oral vaccines that may provide longer and better immunity than the older versions did. If you'd like more information about these vaccines, contact your doctor or local office of public health. Keep in mind that no country requires immunization against cholera as a condition for entry.
References:
https://en.wikipedia.org/wiki/Cholera
http://www.who.int/mediacentre/factsheets/fs107/en/
http://www.cdc.gov/cholera/general/
http://www.tmb.ie/vaccinations/cholera

